Osteoporosis and Spinal Fractures: A Complete Guide to Prevention and Care
Learn how osteoporosis weakens bones and increases the risk of spinal fractures. Discover prevention, treatment, and lifestyle strategies to protect your bone health.


Introduction
Imagine a condition that weakens your bones so gradually you don't feel a thing, until one day, something as simple as bending over to tie your shoes or even a strong cough causes a crack in your spine. This is the reality for millions living with osteoporosis, a "silent" disease that leads to fragile bones and an increased risk of fractures. Spinal fractures, in particular, are a common and serious consequence of osteoporosis, often leading to significant pain, a stooped posture, and a decreased quality of life. But here's the crucial message: these fractures are not an inevitable part of aging. This guide will walk you through everything you need to know about the link between osteoporosis and spinal fractures. We'll cover how to recognise the signs, understand the diagnosis and treatment options, and, most importantly, empower you with strategies for prevention and long-term bone health. Knowledge is your first line of defense.
Understanding the Silent Disease: What is Osteoporosis?
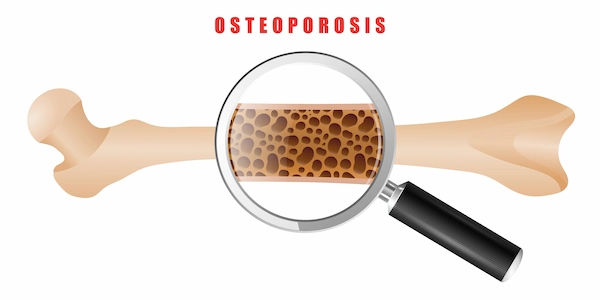
Osteoporosis is a metabolic bone disease characterised by a decrease in bone mass and density, leading to fragile, porous bones that are more susceptible to fractures. Think of healthy bone as a dense honeycomb. With osteoporosis, the holes and spaces in that honeycomb become much larger, weakening the internal structure. This process happens silently and progressively, often without any symptoms until a fracture occurs.
How Osteoporosis Weakens Your Bones
Your bones are living tissue that are constantly being broken down and rebuilt in a process called remodeling. Up until around age 30, you build bone faster than you lose it, reaching your "peak bone mass." After that, bone breakdown slowly overtakes bone formation. In osteoporosis, this imbalance accelerates dramatically, leading to a net loss of bone. Key factors driving this include hormonal changes (especially estrogen decline in menopause), deficiencies in calcium and vitamin D, and a sedentary lifestyle.
Key Risk Factors You Can't Ignore
While aging is a primary risk factor, several others increase your likelihood of developing osteoporosis:
- Gender and Age: Women are at higher risk, especially post-menopausal women over 50.
- Family History: A parent or sibling with osteoporosis or a hip fracture increases your risk.
- Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
- Hormone Levels: Low sex hormone levels (estrogen, testosterone) weaken bone.
- Dietary Factors: Low calcium intake, eating disorders, and gastrointestinal surgery can affect nutrient absorption.
- Long-term Use of Certain Medications: prolonged use of corticosteroid medications (like prednisone) is a significant risk factor.
Consult a Specialist for the best advice
The Link Between Osteoporosis and Your Spine
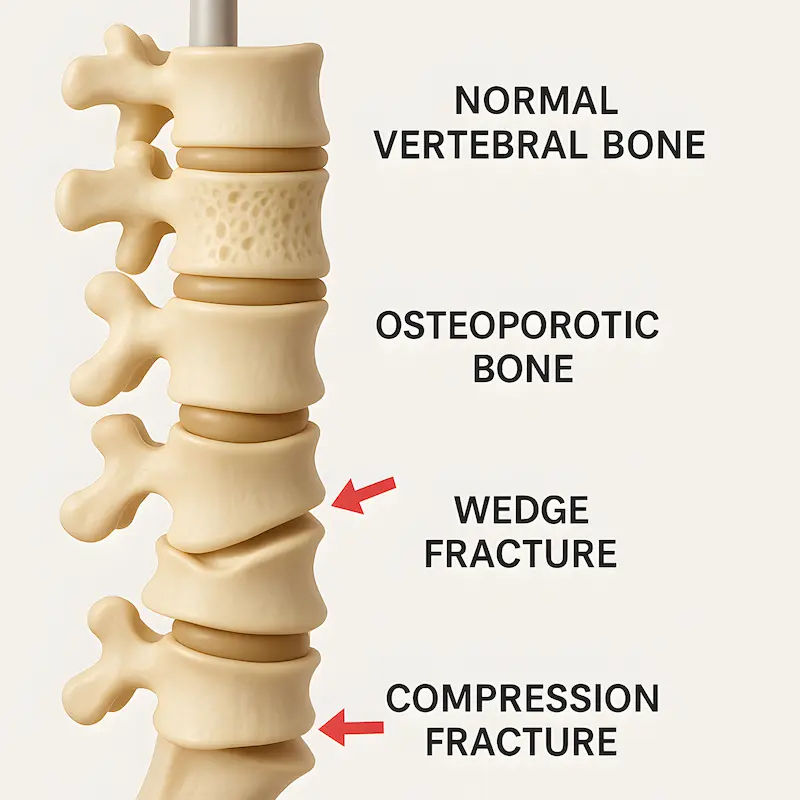
The spine, or vertebral column, is made up of 33 individual bones (vertebrae) stacked on top of one another. These bones are designed to be strong enough to support your body weight but light enough for movement. When osteoporosis weakens these vertebrae, they can collapse under the body's own weight, leading to what is known as a vertebral compression fracture (VCF).
What is a Vertebral Compression Fracture (VCF)?
A VCF is a break in one or more of your vertebrae that causes them to collapse and become compressed, often into a wedge shape. This is the most common type of fracture caused by osteoporosis. Unlike a traumatic fracture from a fall, a VCF can occur during routine activities that put slight pressure on the spine.
How a Simple Action Can Lead to a Spinal Fracture
In advanced osteoporosis, the bones can become so fragile that fractures occur from minimal stress. These are called fragility fractures. Actions that can trigger a spinal compression fracture include:
- Lifting a heavy grocery bag.
- Slipping and catching yourself jarringly.
- A minor fall from a standing height.
- Even a forceful sneeze or cough.
Recognising the Signs: Symptoms of a Spinal Fracture
The symptoms of a spinal fracture can vary dramatically. Some people experience severe, debilitating pain, while others may not feel anything specific.
The "Silent" Fracture: When There Are No Symptoms
Approximately two-thirds of spinal fractures are "silent," meaning they occur without any noticeable symptoms. A person might only become aware of them when an X-ray is taken for an unrelated reason. Over time, multiple silent fractures can lead to a gradual change in posture and height loss.
More Obvious Signs: Pain, Posture Changes, and Height Loss
When symptoms are present, they can include:
- Sudden, Severe Back Pain: Often described as a "grabbing" or "stabbing" pain that worsens with movement and is relieved when lying down.
- Height Loss: As vertebrae collapse, the spine shortens, leading to a measurable loss of height.
- Kyphosis: This is the development of a stooped or hunched posture, sometimes called a
- "dowager's hump." It occurs when several fractures cause the upper spine to curve forward.
- Reduced Mobility: Difficulty bending or twisting due to pain and spinal instability.
Getting a Diagnosis: How Doctors Identify Spinal Fractures
If you suspect a spinal fracture, especially if you have risk factors for osteoporosis, it's crucial to see a doctor. If you experience sudden, severe back pain after a minor incident, consult a doctor online with Apollo24|7 for an initial evaluation to determine the next steps.
The Role of Imaging: X-rays, CT Scans, and MRIs
- X-ray: This is usually the first test ordered. It can show changes in the shape and density of the vertebrae, revealing a collapse.
- MRI (Magnetic Resonance Imaging): An MRI provides a detailed view of the bones and soft tissues, helping to determine the age of the fracture (whether it's new or old) and rule out other causes of pain, like a herniated disc.
- CT Scan: A CT scan provides a more detailed 3D image of the spine than an X-ray and is useful for planning surgical treatment.
The Importance of a Bone Density Test (DEXA Scan)
A dual-energy X-ray absorptiometry (DEXA or DXA) scan is the gold standard for diagnosing osteoporosis. This low-dose X-ray measures the mineral content of your bones, typically at the hip and spine. The result is a "T-score" that compares your bone density to that of a healthy young adult. A T-score of -2.5 or lower indicates osteoporosis. If you are at risk, your doctor may recommend this test. Apollo24|7 offers a convenient home collection for tests like vitamin D, which is crucial for bone health, and can guide you on where to get a DEXA scan.
Treatment Options: Healing and Strengthening Your Spine
The goal of treatment is to relieve pain, stabilise the fracture, prevent future fractures, and treat the underlying osteoporosis.
Non-Surgical Treatments: Rest, Medication, and Bracing
Most spinal fractures heal on their own with conservative care over 6 to 12 weeks, such as:
- Rest and Activity Modification: Short-term rest is important, but doctors will encourage safe movement as soon as possible to prevent further bone loss from inactivity.
- Pain Management: Over-the-counter pain relievers (like acetaminophen) or prescription medications may be used.
- Bracing: A back brace can provide external support, limit painful motion, and help maintain spinal alignment during healing.
Surgical Interventions: Vertebroplasty and Kyphoplasty
For fractures that cause severe, persistent pain despite conservative treatment, minimally invasive procedures may be considered. They are:
- Vertebroplasty: A doctor injects a special bone cement into the fractured vertebra to stabilise it.
- Kyphoplasty: This is similar, but a balloon is first inserted to create a cavity and restore some of the lost height before the cement is injected. This can help correct the spinal deformity.
Living Well After a Fracture: Recovery and Management
Recovery involves both physical healing and adapting to life with a stronger focus on bone health.
Safe Exercises for Strengthening Bones and Muscles
Weight-bearing and muscle-strengthening exercises are vital. A physical therapist can design a safe program, which may include:
- Weight-bearing: Walking, stair climbing.
- Strength Training: Using resistance bands or light weights to strengthen back and core muscles.
- Posture Training: Exercises to improve posture and reduce strain on the spine.
Pain Management Strategies for Daily Life
Beyond medication, techniques like heat/ice therapy, acupuncture, and mindfulness can help manage chronic pain. Creating an ergonomic home environment to avoid bending and twisting is also key.
The Best Defense: Preventing Osteoporosis and Future Fractures
Prevention is always better than cure. It's a lifelong process that starts in youth and continues throughout life.
Building Peak Bone Mass: Nutrition and Exercise in Youth
The best time to build bone density is during childhood and adolescence. Ensuring adequate calcium and vitamin D intake and encouraging regular physical activity during these years sets the stage for stronger bones later in life.
Maintaining Bone Health as You Age: Calcium, Vitamin D, and Lifestyle
Support your bones with proper nutrition, exercise, and healthy habits, such as:
- Calcium: Aim for 1,000-1,200 mg per day from dietary sources (dairy, leafy greens, fortified foods) or supplements.
- Vitamin D: Crucial for calcium absorption. Get safe sun exposure and consider supplements, especially if you have limited sun exposure. A simple blood test from Apollo24|7's home collection service can check your vitamin D levels.
- Exercise: Continue weight-bearing and muscle-strengthening exercises.
- Avoid Smoking and Limit Alcohol: Both can accelerate bone loss.
Conclusion: Taking Control of Your Bone Health
Osteoporosis and spinal fractures can seem daunting, but they are not a fate you have to accept passively. By understanding the risks, recognising the signs, and taking proactive steps, you can significantly strengthen your skeletal foundation. Whether you're in your 30s building peak bone mass or in your 70s managing an existing condition, it's never too early or too late to invest in your bones. Start with a conversation with your doctor about your personal risk factors. Embrace a bone-healthy lifestyle with proper nutrition and regular exercise. By making your bone health a priority today, you are investing in a stronger, more mobile, and pain-free future. If your condition does not improve after trying conservative methods, book a physical visit to a doctor with Apollo24|7 for a comprehensive evaluation and personalised treatment plan.
Consult a Specialist for the best advice
Consult a Specialist for the best advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Brig K Shanmuganandan
Rheumatologist
27 Years • MBBS, MD (Med.), DNB (Med.), Fellow (Rheuma.)
Chennai
Apollo Hospitals Greams Road, Chennai
(475+ Patients)
Dr Ankit Patowari
Rheumatologist
6 Years • MBBS, MD MEDICINE, DM RHEUMATOLOGY
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr. Ramineni Naga Tejaswini
Rheumatologist
3 Years • MBBS, DNB(Internal Medicine), DrNB ( Clinical Immunology and Rheumatology)
Hyderabad
Apollo Hospitals Jubilee Hills Hyderabad, Hyderabad
Consult a Specialist for the best advice

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Brig K Shanmuganandan
Rheumatologist
27 Years • MBBS, MD (Med.), DNB (Med.), Fellow (Rheuma.)
Chennai
Apollo Hospitals Greams Road, Chennai
(475+ Patients)
Dr Ankit Patowari
Rheumatologist
6 Years • MBBS, MD MEDICINE, DM RHEUMATOLOGY
Guwahati
Apollo Clinic Guwahati, Assam, Guwahati
Dr. Ramineni Naga Tejaswini
Rheumatologist
3 Years • MBBS, DNB(Internal Medicine), DrNB ( Clinical Immunology and Rheumatology)
Hyderabad
Apollo Hospitals Jubilee Hills Hyderabad, Hyderabad
More articles from Osteoporosis
Frequently Asked Questions
Can a spinal fracture from osteoporosis heal on its own?
Yes, most osteoporotic spinal fractures will heal with conservative treatment like rest, pain medication, and bracing over 6-12 weeks. However, the bone will heal in its collapsed position, which can lead to permanent changes in posture.
What is the life expectancy after a spinal fracture?
A spinal fracture itself is not typically fatal. However, studies show that suffering a fragility fracture like a VCF can be associated with a decreased life expectancy, primarily due to the related decline in overall health, mobility, and potential complications like pneumonia. This underscores the importance of active treatment and prevention.
What are the best foods to eat for osteoporosis?
Focus on calcium-rich foods like low-fat dairy products (milk, yoghurt), dark leafy greens (kale, broccoli), and fortified foods (tofu, orange juice). Also, include vitamin D sources like fatty fish (salmon, tuna) and egg yolks to help with calcium absorption.
What is the difference between osteoporosis and osteoarthritis?
This is a common confusion. Osteoporosis is a disease of bone density, making bones weak and brittle. Osteoarthritis is a disease of the joints, where the protective cartilage breaks down, causing pain and stiffness. It is possible to have both conditions.
Are vertebroplasty and kyphoplasty safe procedures?
These are generally safe and effective minimally invasive procedures for relieving pain from spinal fractures. As with any procedure, there are risks, such as cement leakage, but serious complications are rare. The decision should be made in consultation with a spine specialist.