Guide to Understanding Osteoporosis Bone Health
Understand osteoporosis, its causes, symptoms, and risk factors. Our comprehensive guide provides actionable tips on diet, exercise, and lifestyle changes to improve bone density and prevent fractures.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. M L Ezhilarasan MBBS
Last updated on 13th Jan, 2026

Imagine your bones as the foundation of your body—a living, dynamic framework that constantly remodels itself. But what happens when this framework weakens, becoming porous and fragile? This silent process is osteoporosis, a condition that affects millions worldwide, often without any warning until a minor fall results in a major fracture. It’s more than just an "old person's disease"; it's a significant health concern that can impact your mobility, independence, and overall quality of life. The good news? Osteoporosis is not an inevitable part of aging. With the right knowledge and proactive steps, you can build resilient bones and protect your skeletal health for years to come. This comprehensive guide will demystify osteoporosis, from understanding your risk factors to actionable strategies for prevention and management, empowering you to take control of your bone health.
What Exactly Is Osteoporosis?
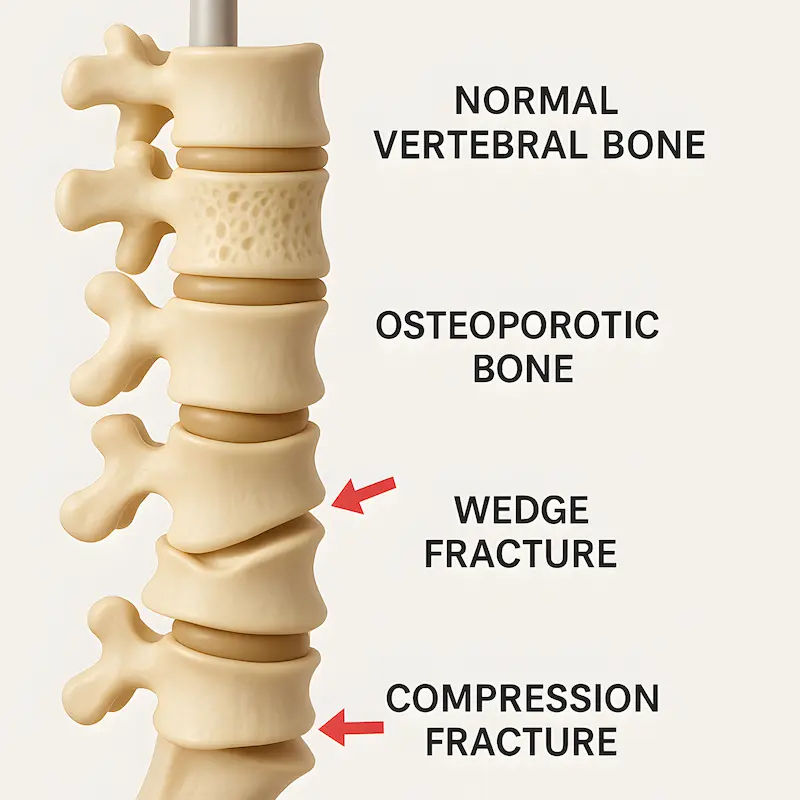
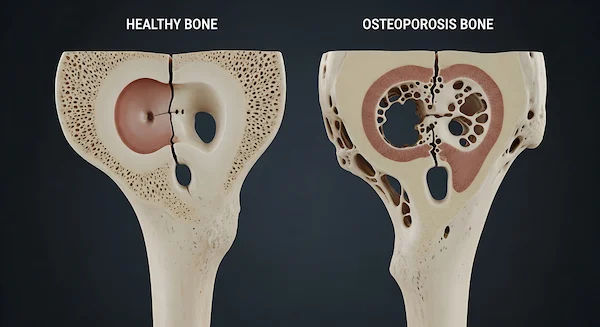
Osteoporosis is a metabolic bone disease characterized by a decrease in bone mass and deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk. Think of healthy bone as a dense honeycomb. With osteoporosis, the holes and spaces in that honeycomb become much larger, weakening the internal structure. This makes bones so fragile that a cough, a slight bump, or even bending over to tie a shoe can cause a break.
The Silent Thief: Why Osteoporosis Often Goes Unnoticed
- Osteoporosis is often called a "silent disease" because bone loss occurs without any symptoms. You can’t feel your bones getting weaker. Many people only discover they have the condition after they suffer a sudden fracture, most commonly in the hip, spine, or wrist. A spinal fracture (vertebral fracture) might manifest as severe back pain, loss of height, or a stooped posture (sometimes called a "dowager's hump"), but these are often mistaken for simple signs of aging rather than an underlying medical condition.
Consult a General Physician for the best advice
Are You at Risk? Understanding the Causes and Risk Factors
Your risk of developing osteoporosis depends on a combination of genetic, hormonal, and lifestyle factors. Understanding these is the first step toward prevention.
NonModifiable Risk Factors (Things You Can't Change)
- Age: Bone density peaks around age 30. After that, bone loss naturally outpaces bone formation.
- Sex: Women are at a significantly higher risk than men, especially after menopause due to a sharp decline in estrogen, a hormone that protects bones.
- Family History: Having a parent or sibling with osteoporosis puts you at greater risk, indicating a genetic predisposition.
- Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
- Race: People of White and Asian descent are at highest risk.
Modifiable Risk Factors (Things You Can Influence)
- Sex Hormone Levels: Reduced estrogen in women (e.g., during menopause) and low testosterone in men can contribute to bone loss.
- Dietary Factors: Low lifetime intake of calcium and vitamin D is a major contributor. Excessive dieting or poor protein intake also hurts bone health.
- Medications: Long-term use of corticosteroid medications (e.g., prednisone), some antiseizure drugs, and others can weaken bone.
- Lifestyle Choices: A sedentary lifestyle, tobacco use, and excessive alcohol consumption (more than two drinks a day) are all detrimental to bones.
Listening to Your Body: Recognizing the Symptoms of Osteoporosis
As mentioned, early stage bone loss has no symptoms. However, once bones have been weakened by osteoporosis, you might notice:
The Most Common Warning Signs
- Back pain, caused by a fractured or collapsed vertebra.
- Loss of height over time.
- A stooped posture or curvature of the spine (kyphosis).
- A bone that breaks much more easily than expected—for instance, a fracture from a minor fall from a standing height.
Getting a Diagnosis: How Osteoporosis is Detected
If you have risk factors or are experiencing potential symptoms of osteoporosis, it's crucial to get evaluated. If you've experienced an unexpected fracture or significant height loss, consult a doctor online with Apollo24|7 for further evaluation.
The Gold Standard: The DXA Bone Density Scan
The most common and accurate way to diagnose bone loss is a DualEnergy Xray Absorptiometry (DXA or DEXA) scan. This low dose X-ray measures your bone mineral density (BMD) at key sites like the hip and spine. Your results are given as a score:
- 1 and above: Normal bone density.
- 1 to 2.5: Osteopenia (low bone mass, a precursor to osteoporosis).
- 2.5 and below: Osteoporosis.
Building Your Defense: Prevention Strategies for Strong Bones
Prevention is the best medicine for osteoporosis. Building strong bones during your youth and maintaining them as an adult is key.
Nutrition for Bone Health: Beyond Calcium and Vitamin D
While calcium and vitamin D are the stars, a balanced osteoporosis diet is crucial.
- Calcium: Adults need 1,0001,200 mg daily. Sources: dairy, leafy greens, fortified foods.
- Vitamin D: Crucial for calcium absorption. Get 600800 IU daily from sunlight, fatty fish, and supplements.
- Protein: Makes up about 50% of bone volume. Include lean meats, beans, and lentils.
Other Key Nutrients: Magnesium, Vitamin K, and Potassium also play vital roles.
The Best Exercises for Bone Density
Bone is living tissue that gets stronger with stress. The best exercises for osteoporosis are:
- Weightbearing exercises: Walking, jogging, dancing, tennis.
- Strength training: Using free weights, resistance bands, or weight machines.
- Balance exercises: Tai chi and yoga can improve stability and prevent falls.
Treatment Options: Slowing Bone Loss and Building Bone
If you are diagnosed, several effective osteoporosis treatment options can slow bone loss and even rebuild bone.
Medications for Osteoporosis Management
- Bisphosphonates (e.g., alendronate, zoledronic acid) are the most commonly prescribed medications.
Monoclonal antibody medications (e.g., denosumab) and bonebuilding medications (e.g., teriparatide) are used for more severe cases.
The Role of Physical Therapy and Fall Prevention
- A physical therapist can design a safe exercise program to strengthen muscles and improve balance. Fall prevention is critical—this includes removing home hazards, improving lighting, and wearing supportive shoes.
Living Well with Osteoporosis
A diagnosis isn't a life sentence to inactivity. It’s a call to action to live smarter and more deliberately to protect your bone health and maintain your independence.
Conclusion
Osteoporosis may be common, but it is not inevitable. By understanding the factors that influence your bone health, you can take proactive, powerful steps to fortify your skeletal system. It’s a lifelong commitment that involves nourishing your body with the right nutrients, staying physically active with bone strengthening exercises, and making smart lifestyle choices. Whether you're in your 30s looking to build peak bone mass or in your 60s focused on preservation, it's never too early or too late to start. Listen to your body, assess your risks, and partner with your healthcare provider to create a plan that keeps you standing strong and living life to the fullest. Your future self will thank you for the foundation you build today.
Consult a General Physician
Your Thoughts?
We hope this guide has empowered you with knowledge about protecting your bone health. What was the most surprising thing you learned? Do you have any personal tips for staying active and eating for strong bones? Share your thoughts in the comments below, and if you found this article helpful, please share it with your friends and family on social media to help us spread the word!
Consult a General Physician

Dr. Manish Mathur
General Physician/ Internal Medicine Specialist
23 Years • MD Physician, MRCP
Delhi
The Medi Centre, Delhi

Dr. Abhishek Gowda
General Physician/ Internal Medicine Specialist
3 Years • MBBS MD General Medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Rajshekar B
General Physician/ Internal Medicine Specialist
36 Years • Gen Med MD
Bengaluru
Six Face Clinic, Bengaluru

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
Consult a General Physician for the best advice

Dr. Manish Mathur
General Physician/ Internal Medicine Specialist
23 Years • MD Physician, MRCP
Delhi
The Medi Centre, Delhi

Dr. Abhishek Gowda
General Physician/ Internal Medicine Specialist
3 Years • MBBS MD General Medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Rajshekar B
General Physician/ Internal Medicine Specialist
36 Years • Gen Med MD
Bengaluru
Six Face Clinic, Bengaluru

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
More articles from Osteoporosis
Frequently Asked Questions
What is the difference between osteopenia and osteoporosis?
Osteopenia is a precursor to osteoporosis. It means your bone mineral density is lower than normal but not yet severe enough to be classified as osteoporosis. It's a warning sign to take action on your bone health to prevent progression.
Can men get osteoporosis?
Absolutely. While it's more common in women, about 25% of men over 50 will experience an osteoporosis-related fracture in their lifetime. Male osteoporosis is often underdiagnosed and overlooked.
What are the best calcium supplements to take?
Look for supplements containing calcium citrate or calcium carbonate. Calcium citrate can be taken with or without food, while calcium carbonate is best absorbed with a meal. Apollo24|7 offers a convenient home collection for tests like vitamin D to check your levels and help determine if you need supplementation.
Are there any natural treatments for osteoporosis?
While prescription medications are often necessary for diagnosed osteoporosis, natural management focuses on the pillars of prevention: a nutrient-dense osteoporosis diet, consistent exercise, avoiding smoking, and limiting alcohol. These should always be done in consultation with a doctor.
How often should I get a bone density test?
If you have normal bone density or mild osteopenia, your doctor might recommend a test every 25 years. If you are on medication for osteoporosis, testing is typically done every 12 years to monitor treatment effectiveness.