Guide to What Do You Need Know About Osteoporosis And Spinal Fractures
Learn the essentials of osteoporosis, its risk factors, and how it leads to spinal compression fractures. Get key information on symptoms, diagnosis, and treatment options.

Written by Dr. M L Ezhilarasan
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Introduction
Imagine a framework so delicate that a simple sneeze, bending to tie your shoes, or a minor stumble could cause it to crumble. For millions of people, particularly post-menopausal women and older adults, this is the reality of living with osteoporosis and the resulting spinal fractures. Often called a "silent disease" because bone loss occurs without symptoms, osteoporosis weakens bones to a point where they become porous and fragile. When this weakening affects the vertebrae—the bones that make up your spine—the consequences can be painful and life-altering. This comprehensive guide will walk you through everything you need to know about the link between osteoporosis and spinal fractures, from understanding the causes and recognizing the symptoms to exploring the latest treatment options and effective prevention strategies. Our goal is to empower you with knowledge to protect your spine and maintain your quality of life.
Understanding the Basics: What is Osteoporosis?
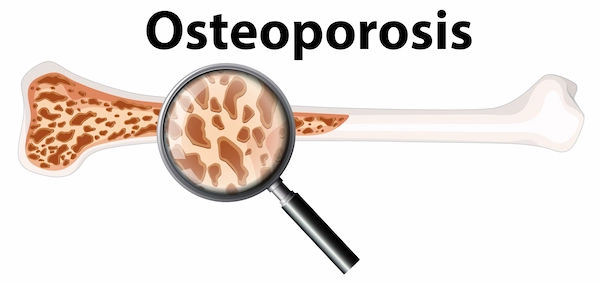
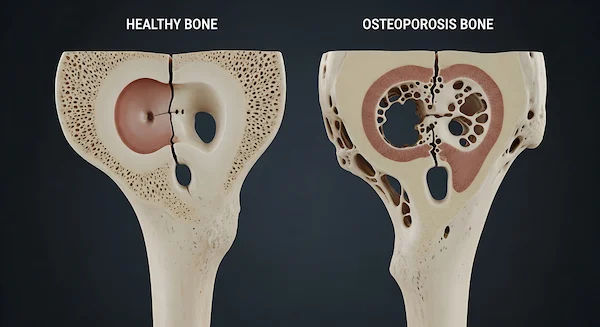
Osteoporosis is a metabolic bone disease characterized by a decrease in bone mass and density, leading to weakened bones and an increased risk of fractures. Think of your bones as living tissue that is constantly being broken down and rebuilt. In youth, bone formation outpaces removal. But around age 30, this process reverses, and bone loss slowly begins. Osteoporosis accelerates this loss, creating holes and spaces in the bone's honeycomb structure, making it brittle.
The Silent Thief: How Osteoporosis Weakens Your Bones
The term "silent thief" is used because bone density is stolen away over years without any pain or obvious signs. You might not know you have it until a minor fall causes a broken wrist, hip, or—most commonly—a fracture in your spine. It’s a progressive condition, meaning the weakening happens gradually, making early detection and intervention crucial.
Consult Top Specialists
The Critical Link: How Osteoporosis Leads to Spinal Fractures
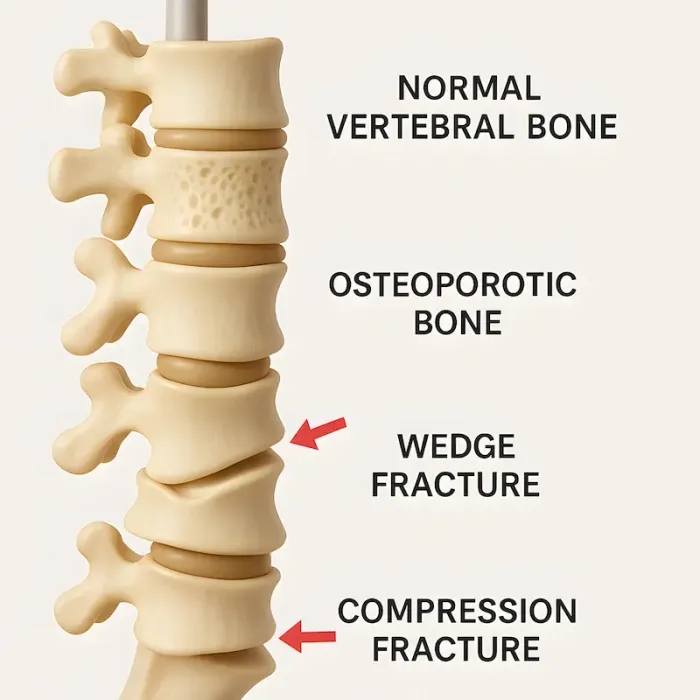
Your spine is a column of 33 vertebrae stacked on top of one another. These bones provide structural support. When they are weakened by osteoporosis, they can no longer withstand everyday stresses. As a result, a vertebrae can collapse or fracture. This is known as a vertebral compression fracture (VCF), and it is the most common type of osteoporotic fracture. In fact, according to the International Osteoporosis Foundation, spinal fractures affect nearly one in two women and one in four men over the age of 50.
Types of Spinal Fractures Caused by Osteoporosis
Vertebral Compression Fractures (VCFs)
This is the most frequent type, where the entire vertebral body collapses uniformly under pressure, losing height. It often occurs in the middle (thoracic) region of the spine.
Wedge Fractures
In this case, the front (anterior) part of the vertebra collapses, forming a wedge shape. This is a common cause of the stooped-forward posture known as kyphosis, or "dowager's hump."
Burst Fractures
Less common but more severe, a burst fracture involves the vertebra breaking in multiple directions. This type can pose a risk to the spinal cord and often requires surgical intervention.
Are You at Risk? Key Risk Factors for Osteoporosis
Understanding your risk is the first step toward prevention. While some factors are uncontrollable, many are related to lifestyle. Key risk factors include:
• Age and Gender: Women over 50 and men over 70 are at highest risk. Women are particularly susceptible due to the rapid bone loss that follows menopause.
• Family History: A parent or sibling with osteoporosis or a hip fracture increases your risk.
• Body Frame Size: Men and women with small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
• Hormone Levels: Reduced estrogen in women (e.g., after menopause) and low testosterone in men contribute to bone loss.
• Dietary Factors: Low calcium and vitamin D intake throughout life.
• Lifestyle Choices: Sedentary lifestyle, excessive alcohol consumption, and tobacco use.
• Certain Medications: Long-term use of corticosteroids (like prednisone) and some other drugs.
If you have several of these risk factors for bone loss, it's wise to speak with a doctor about a bone density test.
Recognizing the Signs: Symptoms of Osteoporosis and Spinal Fractures
The Silence of Osteoporosis
Osteoporosis itself typically has no symptoms. The first sign is often a fracture. However, some people may experience back pain or a noticeable loss of height over time before a fracture is diagnosed.
Tell-tale Signs of a Spinal Fracture
The symptoms of a spinal compression fracture can be sudden and severe or develop gradually. They include:
1. Sudden, severe back pain that worsens with standing or walking and may lessen when lying down.
2. A gradual onset of chronic back pain.
3. Loss of height (often an inch or more over time).
4. A stooped or hunched forward posture (kyphosis).
5. Decreased mobility and difficulty bending or twisting.
If you experience sudden, severe back pain after a minor strain or fall, it is essential to consult a doctor promptly. You can book a physical visit or consult a doctor online with Apollo24|7 for an initial evaluation.
Getting a Diagnosis: How Doctors Identify Bone Loss and Fractures
The Gold Standard: Bone Density Scan (DEXA)
A Dual-Energy X-ray Absorptiometry (DEXA) scan is a low-dose X-ray that measures bone mineral density (BMD). It is painless, quick, and highly accurate. Your results are given as a T-score, which compares your bone density to that of a healthy young adult. A T-score of -2.5 or lower indicates osteoporosis.
Imaging for Fractures: X-rays, CT Scans, and MRIs
If a fracture is suspected, your doctor will order imaging tests. An X-ray can show a collapsed vertebra. A CT scan provides more detailed images of the bone, while an MRI can reveal recent fractures and assess potential damage to nearby nerves.
Treatment Options: Healing and Strengthening Your Spine
Non-Surgical Treatments: Medication and Lifestyle
The primary goals are to relieve pain, stabilize the fracture, and prevent future fractures.
• Medications: Pain relievers, along with bone-strengthening drugs like bisphosphonates (e.g., alendronate) or other agents.
• Bracing: A back brace can support the spine and reduce pain during healing.
• Rest and Modified Activity: Short-term rest is advised, followed by gradual reintroduction of activity under guidance.
Surgical Interventions: Kyphoplasty and Vertebroplasty
For painful fractures that don't heal with conservative care, minimally invasive procedures like kyphoplasty and vertebroplasty can be effective. They involve injecting medical cement into the fractured vertebra to stabilize it and often provide rapid pain relief.
Living Well with Osteoporosis: Prevention and Management Strategies
A diagnosis of osteoporosis is not a life sentence of frailty. With proactive management, you can strengthen your bones and reduce fracture risk.
Building Strong Bones: The Role of Calcium and Vitamin D
Calcium is the building block of bone, and Vitamin D is essential for your body to absorb it. The National Institutes of Health (NIH) recommends 1,200 mg of calcium and 800 IU of Vitamin D daily for adults over 50. Apollo24|7 offers a convenient home collection for tests like vitamin D to check if your levels are adequate.
Essential Exercises for Bone Health
Weight-bearing and muscle-strengthening exercises are vital. The best exercises for osteoporosis include:
• Weight-bearing: Walking, jogging, dancing.
• Strength Training: Using free weights, resistance bands, or weight machines.
• Balance Exercises: Tai Chi and yoga to prevent falls.
Fall Prevention: Making Your Environment Safe
Preventing falls is critical. Remove tripping hazards, ensure good lighting, install grab bars in bathrooms, and wear sturdy, non-slip shoes.
The Long-Term Outlook: Quality of Life and Prognosis
With proper treatment and lifestyle changes, the progression of osteoporosis can be slowed or halted. While existing spinal fractures cannot be reversed, their effects can be managed. The goal is to maintain independence, manage pain, and prevent new fractures, allowing for a full and active life.
Conclusion
Osteoporosis and spinal fractures are serious, but they are not inevitable. Knowledge is your greatest defense. By understanding your risk factors, adopting bone-healthy habits early in life, and seeking timely medical advice, you can build a strong foundation for your skeletal health. If you are concerned about bone density or are experiencing persistent back pain, don't wait. A proactive approach today can prevent a fracture tomorrow. Consult a doctor online with Apollo24|7 to discuss your risk factors and whether a bone density test is right for you. Your future self will thank you for the steps you take today to protect your spine and your independence.Consult Top Specialists
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Mijanur Rahaman Mondal
General Practitioner
3 Years • MBBS
Kolkata
Dr Utsa Basu Clinic, Kolkata
(25+ Patients)

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Mijanur Rahaman Mondal
General Practitioner
3 Years • MBBS
Kolkata
Dr Utsa Basu Clinic, Kolkata
(25+ Patients)

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Osteoporosis
Frequently Asked Questions
1. Can a spinal fracture from osteoporosis heal on its own?
Yes, most spinal fractures will heal over 8 to 12 weeks with rest, pain medication, and bracing. However, the collapsed vertebra will remain deformed, which can lead to chronic pain and postural changes. Procedures like kyphoplasty are considered if healing is slow or pain is severe.
2. What is the difference between osteoporosis and osteopenia?
Osteopenia is a precursor to osteoporosis. It means your bone density is lower than normal but not yet low enough to be classified as osteoporosis. It's a warning sign that you should take steps to prevent further bone loss.
Osteopenia is a precursor to osteoporosis. It means your bone density is lower than normal but not yet low enough to be classified as osteoporosis. It's a warning sign that you should take steps to prevent further bone loss.
Excellent non-dairy sources of calcium include dark leafy greens (kale, collard greens), fortified plant-based milks and juices, tofu, sardines and canned salmon (with bones), and almonds.
4. Are there any specific symptoms of osteoporosis in men?
The symptoms are the same as in women: often none until a fracture occurs. Men are at a significant, though often overlooked, risk, especially after age 70 or if they have low testosterone levels.
5. Can you reverse osteoporosis completely?
While you cannot completely 'reverse' it to the bone density of your youth, you can significantly improve bone density with medication and lifestyle changes. The goal is to strengthen bones enough to reduce fracture risk to a minimum.